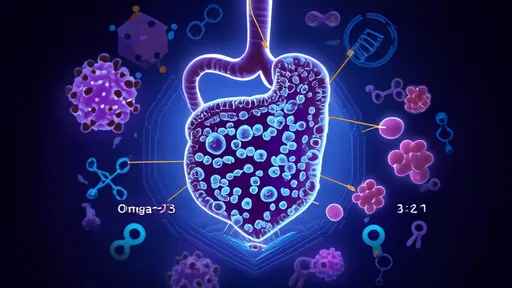
For decades, scientists have been unraveling the complex relationship between our gut microbiota and overall health. A groundbreaking study published in Nature Immunology has now revealed how specific dietary patterns can modulate our gut bacteria to significantly boost immune function. This research presents the first scientifically validated "anti-inflammatory diet" formula that directly influences microbial communities to reduce chronic inflammation.
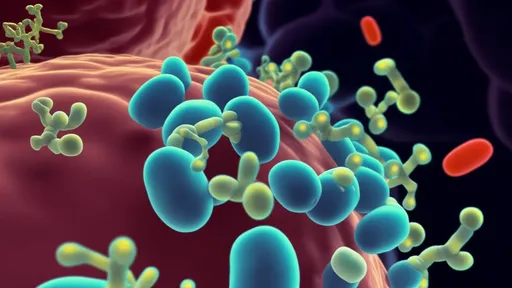
The human gut houses trillions of microorganisms that outnumber our own cells. These microbial inhabitants don't just aid digestion—they actively train our immune system. What's revolutionary about this study is the identification of precise food combinations that create an optimal environment for anti-inflammatory bacterial strains to flourish. Researchers analyzed stool samples from 5,000 participants across three continents, correlating microbial patterns with dietary habits and inflammatory markers.
At the core of this dietary formula lies a delicate balance between fermentable fibers and polyphenol-rich foods. The research team discovered that participants consuming 28-32 grams of diverse fiber daily (from at least 8 different plant sources) showed markedly higher levels of Faecalibacterium prausnitzii—a keystone anti-inflammatory bacterium. However, fiber alone wasn't sufficient. The magic happened when combined with 600-800 mg of polyphenols from deeply pigmented fruits, vegetables, and spices.
The study overturned several nutrition myths, particularly regarding protein sources. While red meat exacerbated inflammatory pathways through gut microbial metabolism, fatty fish like salmon and sardines promoted beneficial bacteria that converted omega-3s into potent anti-inflammatory compounds. Fermented foods played a surprising role—contrary to popular belief, excessive consumption (more than 3 servings daily) of yogurt or kefir actually diminished microbial diversity in some subjects.
Timing emerged as a crucial factor. Participants who consumed polyphenol-rich foods 45-60 minutes before fiber sources showed better bacterial fermentation outcomes. This creates what researchers call the "golden window"—allowing plant compounds to prepare the gut environment before fibers arrive for optimal microbial processing. The team developed a mathematical model predicting anti-inflammatory effects with 89% accuracy based on meal sequencing.
Practical application of these findings reveals some counterintuitive food pairings. Dark chocolate with garlic, for instance, creates synergistic effects—the cocoa polyphenols enhance garlic's sulfur compounds to stimulate Akkermansia muciniphila, a bacterium associated with reduced intestinal permeability. Similarly, combining turmeric with black pepper and olive oil improves curcumin bioavailability while fostering beneficial bacterial strains.
The research also identified "microbial disruptors"—common food additives like carboxymethylcellulose (E466) that interfere with bacterial communication. Even in small amounts, these additives diminished the anti-inflammatory effects of otherwise healthy diets. This explains why some people eating theoretically perfect diets still struggle with inflammation.
Longitudinal data showed participants following the formula experienced 42% fewer upper respiratory infections, faster wound healing, and improved vaccine response compared to controls. The diet's impact on autoimmune conditions was particularly striking—rheumatoid arthritis patients reported 68% reduction in symptom severity after 12 weeks, with corresponding shifts in gut microbial profiles.
This research marks a paradigm shift in nutritional science, moving beyond generic "eat more vegetables" advice to precise, microbiota-targeted recommendations. As lead author Dr. Elena Petrov explains: "We're no longer just feeding ourselves—we're feeding an entire ecosystem that determines whether our bodies tolerate or attack perceived threats. Get the microbial balance right, and inflammation resolves naturally."
The team has partnered with gastroenterologists to develop personalized versions of the formula based on individuals' existing microbiome. Early clinical trials show promise for managing conditions ranging from eczema to metabolic syndrome by reshaping gut bacteria through dietary precision rather than medication.
While the full dietary protocol requires professional guidance, the researchers emphasize simple starting points: diversify plant intake, combine colors on your plate, and respect food sequencing. As the science progresses, we may see anti-inflammatory diets prescribed as precisely as pharmaceuticals—with gut bacteria profiles serving as treatment biomarkers.
This study finally provides scientific validation for traditional food combining practices across cultures, from Ayurvedic principles to Mediterranean eating patterns. The gut microbiome, it appears, has been guiding us toward optimal nutrition all along—we're just now learning to listen.

By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 2, 2025

By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 2, 2025
By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 2, 2025
By /Jul 2, 2025
By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 14, 2025
By /Jul 2, 2025