The world of sports medicine is undergoing a seismic shift as traditional cryotherapy methods for injury recovery are being outpaced by groundbreaking biotechnological advancements. For decades, ice baths and localized cold applications dominated locker rooms and physical therapy clinics, but new research reveals these approaches may delay healing by suppressing natural inflammatory responses. Three emerging biological technologies are redefining how athletes recover from musculoskeletal trauma at the cellular level.
Platelet-Rich Plasma (PRP) therapies have emerged as a sophisticated alternative to blunt-force cold applications. Where cryotherapy numbs pain temporarily, PRP injections harness the body's own growth factors to accelerate tissue regeneration. Sports physicians now isolate platelets from an athlete's blood, concentrate them through centrifugation, and reinject them precisely into damaged ligaments or tendons. This process creates a biochemical scaffold that recruits stem cells to the injury site—something impossible to achieve through surface cooling alone. Recent studies on NBA players show PRP reduces tendon repair time by 40% compared to traditional icing protocols.
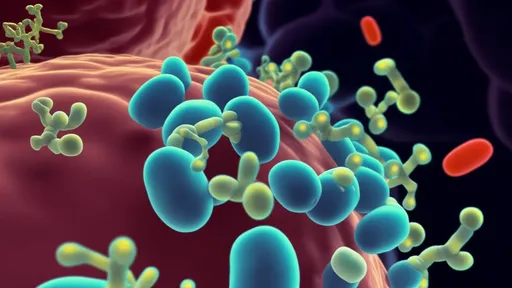
Exosome therapy represents an even more revolutionary approach, particularly for chronic sports injuries resistant to conventional treatments. These nano-sized vesicles derived from stem cells act as biological messengers, delivering regenerative instructions directly to damaged cells. Unlike cryotherapy which merely reduces swelling, exosomes modulate inflammation while simultaneously stimulating tissue remodeling. Professional soccer teams across Europe now use exosome-infused patches that penetrate deeper than cold gels, addressing microtears in muscle fascia that ice cannot reach. The technology shows particular promise for accelerating return-to-play timelines after hamstring and ACL injuries.
The third paradigm shift comes from bioengineered scaffolding matrices that physically bridge damaged tissue while releasing timed doses of therapeutic compounds. These collagen-based structures, often 3D-printed to match specific injury geometries, provide mechanical support during healing—a critical factor absent in passive cold therapies. Professional cyclists using scaffold implants for meniscus tears have demonstrated 30% faster cartilage regeneration compared to peers relying on post-ride ice baths. The matrices gradually dissolve as natural tissue regrows, leaving no foreign material behind.
What makes these biotechnologies fundamentally different from cryotherapy is their proactive engagement with the healing process. Cold applications work against biology by constricting blood vessels and slowing metabolic activity—precisely the opposite of what damaged tissue requires during regeneration. In contrast, the new wave of treatments leverages the body's innate repair mechanisms, providing targeted biological support rather than generalized suppression. Professional sports organizations now invest heavily in these technologies, with some Premier League clubs establishing on-site biotech labs to customize treatments for individual players.
The transition from ice baths to biological solutions reflects a broader philosophical change in sports medicine. Where cold therapy approached injuries as problems to be numbed, modern techniques view them as opportunities to enhance the body's natural adaptive capacities. This paradigm shift extends beyond elite athletes—recent FDA clearances have made several of these technologies accessible to amateur competitors and active individuals. As research continues to validate their efficacy, the days of reaching for ice packs first may soon seem as antiquated as leather football helmets.

By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 2, 2025

By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 2, 2025
By /Jul 2, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 2, 2025
By /Jul 2, 2025
By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 14, 2025
By /Jul 2, 2025